Polypectomy
Polypectomy is a medical procedure to remove abnormal tissue growths called polyps, which can develop in various parts of the gastrointestinal (GI) tract, including the esophagus, stomach, intestines, and colon. The procedure is often performed during an endoscopy to prevent complications like bleeding, obstruction, or progression to cancer.
Types of Polyps
- Hyperplastic Polyps: Typically benign and low-risk for cancer.
- Adenomatous Polyps: Precancerous growths that may develop into cancer if untreated.
- Inflammatory Polyps: Common in patients with inflammatory bowel disease.
- Fundic Gland Polyps: Associated with prolonged use of proton pump inhibitors.
Indications for Polypectomy
- Removal of suspicious or precancerous polyps detected during an endoscopy.
- Treating symptoms caused by polyps, such as bleeding, obstruction, or discomfort.
- Preventing malignancy, especially in individuals with a family history of colorectal or GI cancers.
The Polypectomy Procedure
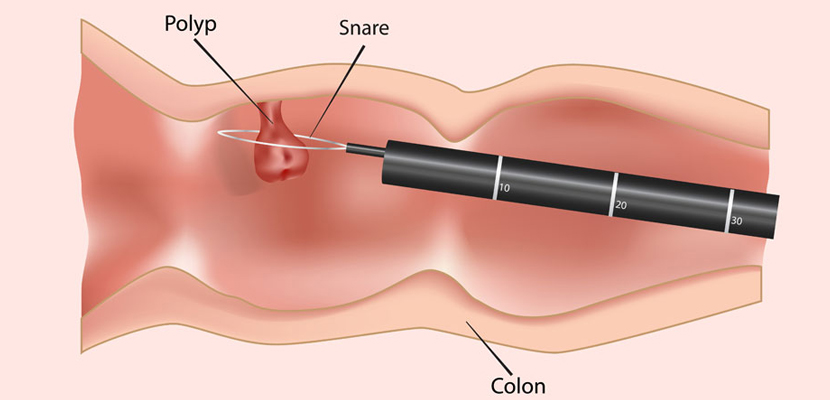
Polypectomy can be performed during an upper or lower GI endoscopy using specialized instruments:
Preparation:
- Fasting for 6–8 hours before the procedure.
- Bowel cleansing for colonic polyps.
- Sedation or anesthesia to ensure comfort during the procedure.
Techniques:
- Snare Polypectomy: A wire loop is used to encircle and cut off the polyp, often with electrocautery to minimize bleeding.
- Cold Forceps Polypectomy: Used for small polyps, where no cauterization is required.
- Endoscopic Mucosal Resection (EMR): For larger polyps, removing part of the mucosal layer to ensure complete excision.
Post-Procedure Care:
- Observation for adverse effects, such as bleeding or perforation.
- Avoiding heavy meals or strenuous activity immediately after the procedure.
Risks and Complications
- Bleeding, especially if the polyp was large or vascular.
- Perforation of the GI wall, which may require surgical repair.
- Infection or localized inflammation.
- Incomplete removal, necessitating follow-up procedures.